
In recent years we have witnessed the growing body of evidence in the field of neuroplasticity. Research has demonstrated that the adult human brain can continue to form neural connections and can grow new brain cells in response to learning or training even into old age (1). Emerging research is now showing that thinking about exercise (mental effort) can result in physical changes to your mind and body.
The technique is called mental practice (MP) or motor imagery (MI). MI has been used by elite athletes and by other disciplines exploring the potential importance of MI within their respective fields. These include psychology, education, medicine and music.
MI has been shown to be crucial for motor skill learning in a variety of situations, ranging from learning new skills in sports (2,3) to overcoming the effects of neurological conditions (2,4,5). Research has found residual cortical activity in motor areas in paraplegic individuals (6) and stroke victims (7) while engaging in imagery.
MI is a mental process by which an individual rehearses or simulates a given action in his/her mind without physically performing the movement (7).
Neuroscience is finding the combination of MI training with physical practice to be more effective than physical practice alone (8).
There is now compelling evidence that MI and actual movement share common neural substrates (9). Brain imaging studies have shown that MI induces similar electroencephalographic (EEG) patterns and activates a brain network that overlaps with that activated by real execution, but the overlap is incomplete (9). See Figure 1.
Should motor functions be damaged, similar impairments would emerge in simulated actions. However, the available studies are largely contradictory. Disassociations have been found dependent upon the type of task, the state of the imager’s motor system, which hemisphere of the brain is involved and extent of the brain damage (10).
Figure 1. Studies investigating the electromyographic (EMG) activity during motor imagery (9)
 activity during motor imagery.jpg)
Interestingly, dependent upon the extent of motor damage, some research participants have been shown to apply alternative strategies to MI to reach a solution. These have included deriving their responses from mentally recalling partial motor information (motor memories) or by handling a visual-spatial image of the action (a representation of the action as it would be if observed) (10). These findings indicate that the notion of MI should be expanded to include processes that are not limited to simulation but also rely on creative operations. “These alternative modes would support the brain’s creative potential to invent novel motor patterns, tools and machinery, and evidently, the ability to imagine what may never be achieved in reality” (10).
Other studies have demonstrated that activated regions of the brain differ depending on the type of MI (i.e. kinaesthetic and visual motor imagery). Activity in the parietal regions was similar between kinaesthetic and visual motor imagery but differed between motor and visual regions (9,11). Therefore, the instruction to participants involved with MI experiments is advised to be explicit and the type of MI desired clearly characterised (11).
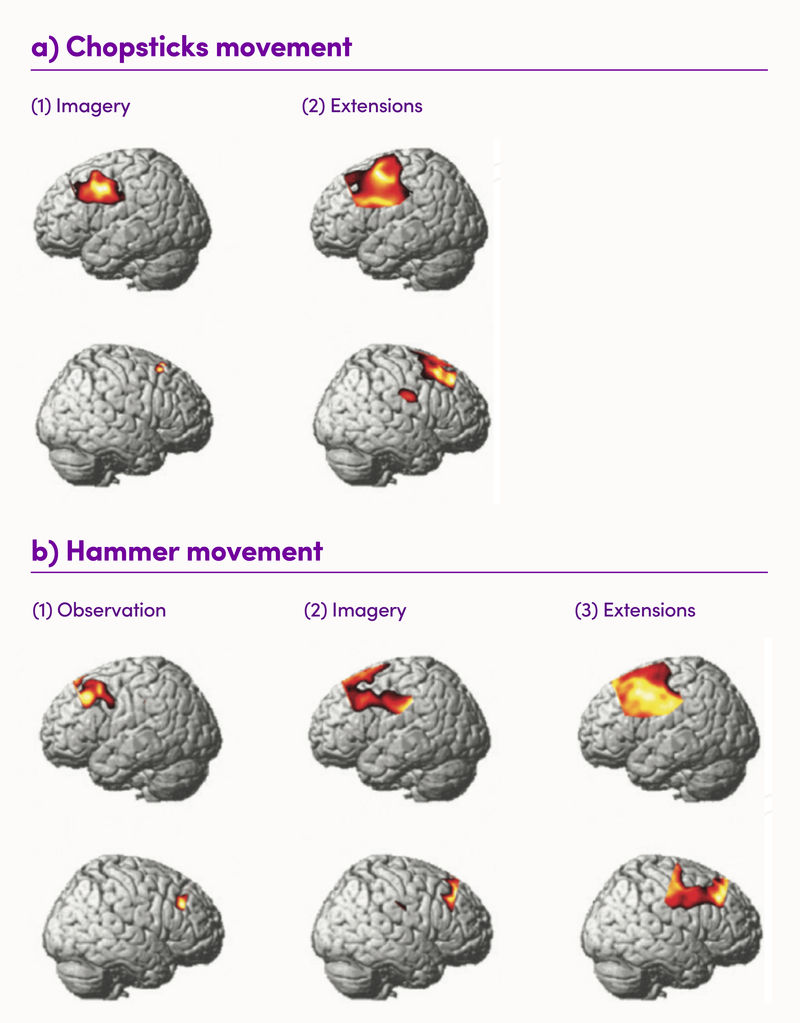
A recent study observed brain activity during observation, imagery and execution of tool use, shown in Figure 2 (12).
Figure 2: Brain activity during observation, imagery and execution of tool use (12). The top row of the images show the left side of the brain, whereas the bottom row of the images show the right side of the brain. (a) Brain regions where a significant increase in the Oxyhaemogolbin (OxyHb) levels was detected during imagery and execution of the chopsticks movement. No significant differences in the oxyHb were detected during observation of the chopsticks movement. (b) Brain regions where a significant increase in the oxyHB levels was detected during observation, imagery and execution of the hammer movement
Some research to date:
- In a randomised controlled study involving patients with complex regional pain syndrome (CRPS) the upper extremity after a wrist fracture, patients received conventional treatment or a motor imagery program (MIP). At 6 and 12 weeks after completion of six treatments, the patients in the MIP group had significantly less pain and decreased swelling. Researchers concluded this treatment modality is promising but requires further investigation (13)
- A randomised controlled study was conducted to compare the effectiveness of pain and upper limb function of mirror therapy on CRPSt1 of the upper limb in patients with acute stroke. 48 patients with CRPSt1 of the affected upper limb were enrolled with a 6-month follow-up and assigned to either a mirror therapy group or placebo control group. Mirror therapy effectively reduced pain and enhanced upper limb motor function in stroke patients with upper limb CRPSt1 (14)
- In 2016 a small study entailed giving participants a mental exercise to perform five days a week for one month and testing the strength of their calf muscles by using force to push hard with their legs against a machine. Ultrasound was used to take a reading of muscle size and mass before pulsing an electrical current through to measure how much muscle they were using. Participants were to imagine themselves pushing against the machine and imagine feeling their muscles contract at least 50 times, for 15 minutes five times a week whilst not actually moving a muscle. 4 weeks later, participants performed the same three tests. Strength improved by an average of 8%, while one participant’s strength increased by 33%. All participants increased using their muscle fibres from 50% to 70%. The growth of muscle did not occur but improvement was found in the quality of muscle (15)
- In another study, 29 volunteers wrapped their wrists in surgical casts for an entire month during which half of the volunteers thought about exercising their immobilized wrists. For 11 minutes a day, 5 days a week, they sat completely still and focused their entire mental effort on pretending to flex their muscles. When the casts were removed, the volunteers that did mental exercises had wrist muscles that were twice as strong as those that had done nothing at all (16)
- A prospective cohort study found that patients with traumatic brain injury (TBI) demonstrated a relatively preserved MI ability, indicating that MI could be used to aid rehabilitation and subsequent functional recovery (17)
Takeaway on Motor Imagery
- MI is a complex phenomenon. A number of studies have confirmed that mental rehearsal can be beneficial for motor learning and suggest that imagery might be used to supplement or partly replace physical practice in clinical rehabilitation (8)
- Although some of the existing evidence is limited by poor trial designs (18), a systematic review in the field of medicine suggests that motor imagery provides additional benefits for functional recovery and could be used to aid rehabilitation (17,18,19)
- Larger and more methodologically sound studies should be conducted to assess the benefits of motor imagery (18)
- The potential for neuroplasticity is widespread and inspiring. Further studies are being conducted within their respective fields






