Listen on Amazon music | Apple Podcasts | Google Podcast | Spotify
Wendy McLean (00:05): Welcome to Common Ground, a podcast series discussing new research and interesting projects in the field of complementary medicine. Hello, my name is Wendy McLean, Senior Writer & Presenter at vital.ly.
vital.ly is a digital platform, a health professional resource, and a distribution service all in one.
Firstly, I'd like to begin by acknowledging the Gadigal people of the Eora Nation as the traditional custodians on the land on which we gather here. I would also like to pay my respect to their elders, both past, present, and emerging.
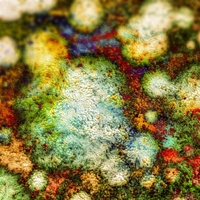
Today on Common Ground I’ll be speaking with Clinical Naturopath Lisa McDonald on Chronic Inflammatory Response Syndrome (CIRS)/Mould illness.
Lisa is also an academic, lecturer and Practitioner Board Member of the Australian Register of Naturopaths and Herbalists (ARONAH) in Australia. Lisa has a Bachelor Degree, majoring in Psychology from Macquarie University and a Masters of Management from Macquarie Graduate School of Management. She gained her naturopathic qualifications at Nature Care College and is currently completing an Honours Degree in Medicines Management, Complementary Medicine at the University of Tasmania.
After personal experience with Chronic Inflammatory Response Syndrome (CIRS)/Mould illness, Lisa became passionate about knowing all there is to know about CIRS/Mould illness and all the confounding health issues that tend to come with patients who experience CIRS and chronic illness. She is one of the few naturopaths in Australia who has studied with Dr Shoemaker and has developed a unique process of analysis of patient’s health to capture, track and treat multisystem illness like CIRS.
Lisa brings together her knowledge of nutrigenomics, psychology, functional medicine, Dr Shoemaker’s and other CIRS thought leaders into her own unique integrated naturopathic systems-based framework to provide individualised treatment.
Over the past decade, Lisa has supported hundreds of patients with CIRS/mould illness, chronic fatigue, anxiety, fertility, mast cell activation syndrome, tick borne and biotoxins related health issues. Taking an approach of blending traditional medicine and the latest science, Lisa takes a highly individualised approach and is passionate about finding the root cause of illness.
She currently runs her own Naturopathic practice from Wallumettagal Country in Sydney, Australia and is an Academic Lecturer at Endeavour College of Natural Health in Australia. She is a founding member of the International Society for Environmentally Acquired Illness (ISEAI) and a Practitioner Board member of (ARONAH).
Welcome to Common Ground, Lisa. It's great to have you here today.
Lisa McDonald (02:40): Thank you so much. I'm really excited to be here.
Wendy McLean (02:43): It's such an important topic and one that you personally have experienced. So perhaps you could start off and share with us a little bit about your background and what led you to specialising in CIRS.
Lisa McDonald (02:55): Oh, look you know, I guess I've always wanted to be a naturopath since I was, you know, a teen. And before I journeyed there, I did do a psychology degree and a master's of management. I worked in global organisations doing mergers and acquisitions and so on all the while I was studying naturopathy on the side. And so I guess once I met all my goals in that kind of world I pivoted and started my own practice as a naturopath and been doing that ever since. But I guess 10 years ago after my son was born, I was experiencing various symptoms. I thought it was just postpartum issues or maybe I was just tired or because my son was so unwell. But over time I had more and more symptoms. And I just couldn't shake them no matter what I did, I did a lot of my naturopathic stuff and I couldn't work out what it was and it kind of really crept up on me because to be honest, I was actually much more focused on my son.
And so he had the world's worst eczema you've ever seen, head to toe. It was relentless. He had nights of weird breathing. He would react to most foods. And that included just being in the same room as when somebody was cooking certain foods. So I guess in hindsight, probably he had a bit of mast cell activation. And my daughter had a few things too. She had food intolerances, gut problems and you know, one or two times she had like all this significant hair loss to the point where there were clumps in the bottom of the swimming pool. So there was lots of stuff. So, you know, for the peak, I guess I was kind of fixated on, you know, worried about my children. And so for my son, for example, the peak for him where he actually became anaphylactic and he had his first anaphylactic reaction by the time he was two where his face blew up into what looked like the elephant man, this purply-white, terrible thing with little dots for eyelashes.
Lisa McDonald (04:51): It was horrible. And we didn't have an EpiPen and fortunately the ambulance came there in time, so his first few years was probably all consuming. And he was so bad that people used to come up to me and either offer advice or they would pull their kids away from them. I've had one person actually say to me once, how irresponsible I was bringing a child with chickenpox into the public, so it wasn't fun. So meanwhile, while all this was happening, I was probably getting more and more symptoms, but I kind of didn't notice because I was more consumed by my son's ill health and all his allergies, et cetera.
Lisa McDonald (05:39): So I kind of was ignoring myself in a lot of ways, but what was happening was that I was getting bouts of extreme fatigue, I was forgetting stuff. My energy would drop during the day, I'd get eye floaters in my eyesight. My memory was shocking. I’d get this numbing and tingling in my hands, dizziness, so it kind of like progressively happened over time. So it's a little bit, can't find the right word, but it kind of like, it sort of creeps up on you. And you know, being a naturopath, you know, still having some symptoms you say, oh, well maybe it's this, maybe it's that. So, I thought it was sugar dysregulation, so I'd try to eat consistently through the day. I thought it was thyroid. And then I sort of got really overwhelmed by small things and I would get cranky a lot.
Lisa McDonald (06:29): So what we kind of call mould rage, but yeah, I would get cranky a lot. And so still none the wiser of what's going on. And I guess I never really considered if there was any sort of environmental issue because wherever we ate organic food. We grew our own veggies. We used low tox/no tox personal products and cleaning products. And even when we renovated our house, we installed like a low VOC kitchen. We did low tox paint. So the thought of our house that could possibly make us sick wasn't even on the radar. But in the meantime, of course we started getting mould growing on the walls in the bedrooms, in the living rooms. And I guess I kind of like cringe about it now when I think of it, but back then I'd think it's a bit of mould, you just wipe it off.
Lisa McDonald (07:36): But it got worse. So, I was doing things back then, which is actually the worst thing you could do. Which I know now, but I didn’t know then, I would put the fans on in the bedrooms and I would wipe all the mould off the walls with a strong mix of vinegar and clove oil thinking that, oh, well, that’s the best way to do it because it’s natural and it’s not chemicals and blah, blah, blah, but it’s not. So of course, the mould spread and pretty much it would grow back in like the wipe marks of like where I had actually tried to wipe it off. And then, even worse because the fans were on that drew all the spores up onto the ceiling. And so I had this lovely pattern of mould starting to grow around the fan where that was. So we had it going on.
Wendy McLean (08:30): That just sounds like a really stressful time. And as you said, you're being so sick as well, yourself. You're not fully across and thinking of these things like the mould. So I guess how difficult was it for you to actually receive a diagnosis of CIRS and how were you able to discern it from other potential things you've already mentioned, blood sugar, thyroid?
Lisa McDonald (08:56): Yeah. Well, I guess at the time I was really searching a lot to try and figure out what was wrong with my son. So part of that was Googling, at all hours at the night. So after Googling and trying to make sense of what was happening with him, I actually came across Dr Shoemaker and the whole mould thing. So I started to look at his work and I vaguely considered the mould, but to be honest, I was probably in denial. It was kind of like, yeah. Okay. That's interesting. But you know, because back then, I mean, this is a long time ago. This is, 10 years ago kind of thing, you know, it wasn't something there was things around black mould maybe. But that was it. And so I was kind of like, mmm, that's interesting, ah, in denial, you know, kind of thing.
Lisa McDonald (09:50): But because it is such a huge thing to consider that your home, where you live and you've invested in it and emotion, to think that your home is making sick. But look, I was really lucky. Fortunately, Dr Shoemaker came to Australia and I signed up for the practitioner training. And so at the time there was really just a group of integrated GPs, a couple of naturopaths and myself, and that was pretty much it. And we did the training. So apart from Dr Sandeep Gupta, who I think has kind of had done his certification around that time, there really wasn't any practitioners to see that were across it at the time. And so we're all kind of learning together. And so, you know, I guess the benefit in a kind of a way was that I kind of learned by trial and error a lot.
And it also meant that I learned that I really needed to think about what Dr Shoemaker had to offer. And now, down the track, we've got other thought leaders as well, because really you can't, you know, I was doing a lot of things naturopathically, but I was still living with? mould. Then getting through the training was really challenging because there was a lot of reading and a lot of one-on-one sessions with Dr Shoemaker and there wasn't really a structured course or webinars or anything I could just log in and learn about. And so I had to, it was a hard yard and of course my brain was a bit mushy because I was breathing in mould. In terms of a differential diagnosis at the time, well, I guess I had already ruled out other things. It was multi-system, it was multi symptom, I'd ruled out other things and frankly, we were living in a mould pit. I have got old photos on an old computer somewhere, but sometimes I can't even look at that because it's actually horrific, but anyway, so, you know, that's how I got there.
Wendy McLean (11:44): Yeah. And that just sounds, it does sound horrific. And you know, a real challenge, as you said, when you're suffering from that brain fog and you're trying to assimilate all this new knowledge. So what were some of the steps that were involved in your recovery and was it a quick process, slow process? How did you go about it?
Lisa McDonald (12:05): Well the key thing was to get out of the house. And so this is the big, and probably the most challenging thing that for most patients particularly because your brain's mush and everything's really overwhelming so that the thought of having to organise and plan a day and your cognition and memory is so poor that, trying to get your head around things is really big. So the smallest things can seem like this massive mountain and you are also really slow to sort of process, slow to do things, it's the weirdest thing. It's almost like being, I don't know, drunk and with dementia, it's kind of bizarre. And extreme fatigue. And of course there's the emotional side of attachment to your things in your house, et cetera.
Lisa McDonald (12:55): So that house for us, for example, had been in our family for since the 1950s, it's where my mum grew up. You know, I had lovely memories with my grandmother because that was my grandmother's house originally. And we had we wanted to knock it down and have a self-sufficient home. Like we had all this emotional attachment to the place, but getting out of the house was super hard because it was at the time when Sydney's housing prices was going up literally a hundred grand a month, you know? So it took 18 months to get out of there. And what I say to patients now and which I, if we all knew what we know now back then, I would've said to me, get a tent and pitch it in the backyard and go and sleep in the tent.
Lisa McDonald (13:37): Like, you know, if I knew it was going be that long. Of course, there's always challenges with trying to find a safe place to move to and the thing about getting away from the mould is often people want to do remediation and, we'd looked at that because we did have it all over the walls, et cetera. And we did spend a lot of time meanwhile trying to work out where the moisture was coming from. Because the key thing is it's actually finding out where the water's coming from and the moisture and what's actually causing the building to be water damaged or having such high humidity in the home.
Lisa McDonald (14:20): And we tried everything. Like we checked all the sewage pipes, and there was still this dampness coming out and, in the end, in the few weeks, as we were sort of starting to want to sell our house there was this water that sort of was seeping up at the back end of our house. So we're kind of like on a gently sloping property. I looked at? it and I think that's weird, this water's coming up, right at the back of the property. And I had that rainbow swirl on top. Clear, but the rainbow swirl which is sewage. Anyway, the long and the short of it is after we spoke to Sydney Water and they came out and had a look, there was actually a massive sewage pipe in the property behind us, which is one of those six foot down, six-foot-high pipes, like the town sewage.
There was this person hole? Man hole? at the property behind us. And it had, and over the years it had caved in because they'd built a veggie patch or something over the top of it. It had blocked the sewage pipe and then the sewage pipe had cracked and all those, all that time, it had been leaking into the soil. So this moisture under the house was this terrible soup of sewage. So anyway, by that stage, we'd already decided we're moving. We were already looking at place we'd already, you know, moved on in a lot of ways. But we left the mould visible in our house so that when the person who bought it, they knew it was basically going to be a knockdown.
So, I don't have any bad vibes about that, but the other thing too about these things is that, in hindsight, I probably should have sued Sydney Water because they basically ruined our house, but your brain is so mush, the cognition stuff is such a challenge, that I didn't even occur to me. So anyway, we ended up finding another house and then I was on the road to recovery.
Wendy McLean (16:26): Oh, that's a horrific story and journey, but I'm glad that you got out, you got into a new place, but once you're in the new place, was there anything that set back your recovery? Was there anything that you did that you shouldn't have? Was there re-exposure to mould?
Lisa McDonald (16:44): Yeah. look well look, I made lots of mistakes, where do I start? Because, remember back then we didn't, I didn't have practitioners or anyone to talk to and, you're sort of building on whatever knowledge and sort of acquired from the education you had to that stage. And I think like a lot of patients there is this element of denial, like you, you know, and so is it really true or is it not?
Wendy McLean (17:09): Yes. Understand.
Lisa McDonald (17:12): So, and look to be honest, I wish I could go back and give myself some advice, but even then, I don’t know if I would listen because it's like crazy lady stuff. So, I guess, we moved out and what I didn't really quite get, was thinking I could treat the mould myself with vinegar and clove oil, which is not a good idea. The other biggest mistake was actually taking a lot of contaminated belongings with us, which I didn't quite realise what that, what contaminated meant. And so thankfully, you know, we got rid of the stinky couch and stuff like that because things were starting to smell. And then anything that had visible mould on it, but what I didn't really truly understand is the things that are like soft furnishings, and books.
Lisa McDonald (18:00): So, you know, I took books, I took my clothes, I took leather stuff, all the things that you really shouldn't. Clothes you can work on. But I had, you know, I had like this awesome collection of books that I'd been collecting, Aboriginal rare books about Aboriginal culture and herbal medicine and so on. So it just didn't occur to me to do anything with them. So I took that with me. And what was really lucky was that because we were in between houses, we put most of our belongings in storage. And so when we moved into our new house, which I knew was safe, and they were in storage for a period of time mould grew on stuff. So when it was coming in, I was just standing the front door and sending it back out.
So the poor removalist, I think the neighbours must have thought we were crazy. Because who were these people who have just moved in, and half their stuff is on the front lawn. It's crazy. So yeah, and you know, we settled in and look, thankfully I had actually put our books, my books in, well, thankfully not thankfully, but I'd actually put it into a separate dwelling. That was, I was using as my clinic, which was pristine. My clinic was white and it looked fantastic, smelt fine. It had like, an air purifier is probably a strong word, but something to try and prevent if anything was going happen. And I had all my books in there, so we are great. We've sort of moved into our new place. We're already on the mend anyway because we've got out of it many months before. But then, you know, I don't know how, I couldn't even tell you how long it was. It was like six months to a year before I really kind of noticed. But so of course, you know, I contaminated my clinic, didn't I with all my books. So I started to get symptoms again, but they were a little bit different. They were more like numbing and stuff on my fingers and things like that.
So there's been quite a few ups and downs in terms of working out, realising especially about your home contents. So I guess and then I address that. So basically all my books and everything had to either go and or I've put ones I can't replace into sealed plastic containers never to be seen again. But unless I'm outside fully gloved up like a crazy person. So one of the things I often say to patients is look, you know, I know it's really overwhelming to move out, et cetera, but one of the, you know, and also to sit there and have to think it's overwhelming to even think about having to sit there and sift through a bookshelf as to what books you'd keep and what books you wouldn't like. That even just little things like that. So overwhelming when you are mouldy for support of a better term. And so I just say to people, look, just put everything into a really good sealed plastic container and put it in a separate dwelling. And when you feel better, go back then, and have a look.
Lisa McDonald (21:14): Yeah. And it's a really important message because at the time no one wants to let go of this stuff that, you know, often people want to hold onto things and it's not until when you feel better and you go, oh my God, I never want to feel like that again. Then people will have a look at their stuff and go, do you know what, I don't really need that? So, yeah. It's a bit of a journey. And then of course, you know, when you're sort of in day-to-day life you just have to be a little bit vigilant about where you go and what you do.
Wendy McLean (21:45): Yeah. That's right. You know, it's home, it's a workplace, these things you need to consider. And I mean, unfortunately at the moment, we're facing this mould epidemic in Eastern Australia with this rainfall this week again, flooding for fourth time in some places. So when is mould an issue? is all mould an issue or are there particular people that are more at risk of developing CIRS and mould related health issues?
Lisa McDonald (22:13): Look, that's an interesting question. I mean, there's certainly some people that are more vulnerable to CIRS or chronic inflammatory response syndrome than others. But you can also have other things, you can also have an allergic response to the mould and you can have what we call colonisation. So you can pick up things that like aspergillosis, which is lung infection caused by exposure to a very common mould, Aspergillus. So there's a number of things that can happen to people when they're exposed to mould. And looking at those that are more susceptible to CIRS is really based on a lot of the work that Dr Shoemaker did. And that's really looking at the HLA DQ/DR gene haplotypes from the work that he's done. But in practice, I have seen people who also can have CIRS not necessarily having that susceptibility, but I'd have to say 99% of my patients do have those genes.
But of course, I'm looking at a skewed proportion of the population because they're coming to me for mould issues in the first place?, as opposed to someone who might be out there in clinic and seeing other types of patients. But yeah, so there's definitely some susceptibilities and I think the other thing is, is that I think previous exposure adds to the pot. I think if people have had previous significant trauma, if they've got a viral load, like Epstein Barr virus, if they've had stealth infections and if their bucket's kind of already full. And it becomes a kind of little bit of a storm, right. So it's kind of like sometimes there might have been some things bubbling along and then they get in a situation where they're exposed to mould and that's just tipped it all over the edge.
The important thing is that to know as a practitioner, is that not everyone in in the household can be affected. So you can have a whole household of people, four people and one person is like absolutely flawed, significant fatigue, you know, can't function. And then the rest of them aren't too bad and maybe one or two have a few respiratory or sinus issues and maybe another one's got a bit of eczema; you know what I mean? It's kind of like, it's not necessarily the entire household that is going to be affected. And so the problem with that is, is that then there's this issue around validation and people feeling like they're mad or people thinking they're mad and/or not getting support of other people in their household to actually make, do the changes that need to be made to that household to actually make them better.
Wendy McLean (24:49): That would be a real problem. And I'm just wondering as well in your clinic, are you seeing people with COVID and mould related issues and are they suffering more, would you say, or potentially suffering from long COVID?
Lisa McDonald (25:07): Yes. I am starting to see people coming in who have got a combination of long COVID. The jury’s out for me onto what extent that those that have a susceptibility to CIRS necessarily are more susceptible to COVID or not. Because if I look across my whole patient base, I haven't necessarily seen all the people who've got CIRS or having long COVID. I'm seeing a handful of people getting that. And coming through the practice. And again, it's interesting looking at, you know, and there's more work, I think we need to do on ? defining what long COVID looks like. I mean, obviously the World Health Organisation does have a set of criteria, but also on the ground, you know, if any of you have done any sort of the training around at the moment of what we're seeing in practice, you need to take in consideration.
And then we kind of think, well, differential diagnosis between that and Epstein Barr virus, which also often comes with it. And stealth infection and CIRS, so I think I would just look at it in terms of it's part of the melting pot and the storm that you might see with a CIRS patient and consider all those things and, you know, we're holistic practitioners. So that's our job is that we hold it all and then we work out, okay, what is it that we need to do to support this, that it's not about just one diagnosis often it's a cluster of things.
Wendy McLean (26:37): Yeah, absolutely. That's right. And you've talked about looking at, say genetic markers. So is there other testing that you do to go about diagnosing CIRS?
Lisa McDonald (26:49): Yeah. So look, I think in terms of the diagnosis for CIRS, I think really the important message is there is no one test for CIRS out there. It's really important that it's at this stage, it is a combination of a clinical analysis, clinical presentation, and some testing. So clinical presentation would be meeting the symptom clusters that Dr Shoemaker came up with. We also see other things as well as part of CIRS, but they're kind of like your baseline. And that you've done really good clinical case taking, that you've done a timeline. So you've looked back and said, okay, tell me about this. You know, X, Y, Z, tell me about the fatigue. When did that start? Where were you living at the time?
So there's the timeline of like, what was their environment at the time is when some of the symptoms started to occur. And so it's really good case taking as well. And then also you, we can do some of the… so there is Dr Shoemakers tests and their biomarkers. And again, they're not perfect nor can you look at them in total, one of them in isolation, you need to do a couple of them to look at the pattern of results, because they're kind of just picking up some expressions of what some of the innate immune system or the cytokine storm that happens may expressed in someone's body. But they're all, you know, some of those markers are also for other things. So for example, leptin on its own is not going to be useful because leptin can also be elevated with metabolic issues, et cetera, not necessary just because they've been exposed to mould.
So you have to look at some of the other biomarkers and if you go to my website there's information about those there. Or even Dr Shoemaker’s information. But some of the things that the challenges we have in Australia is we can't do all those biomarkers. We can't accurately get those biomarkers done in Australia. So there's some that we can do. And some that we can't. The ones you can do in most labs across Australia and the mainstream labs are things like leptin and vasointestinal peptide, and copeptin and osmolality, they're kind of like the key ones you can usually get. We can also test for the HLA DQ/DR genes and looking at those haplotypes. Remembering that genes are not a diagnosis, genes are just a susceptibility.
And also remembering that a lot of the gene haplotypes have been based on Dr Shoemaker’s work. So there's not a significant, and there, hopefully there will be overtime, but, you know, it's not based on one piece of research, it's based on a lot of clinical data. And then of course they need to have been exposed. And sometimes that's hard to unpack because people go, oh, no, I don't have mould at my house. So there's also really good questioning around you know, have you had any leaks in your home? Has there been any flooding? What do you understand about the history of that home? Because obviously they're not necessarily going to be the first people that have lived there. So I even ask questions around the topography of the lands that they're on and, and what happens when it rains?
Lisa McDonald (30:07): Does the water go under your house or does it go around your house? It's even like some of the drainage and stuff, so you have to be like a sleuth. So, and then of course you have to test those things to rule it, other things out. So being, and it needs to be multi-system and multi symptoms. So just because they’ve got significant fatigue, that doesn't mean they have CIRS because they need to have, they need to have significant fatigue plus other things. It's super important to have a look at the whole piece. And that's why I think practitioners like naturopaths and integrated GPs we tend to look at things holistically and look at all those things. We have the time. And also the other thing too, is not just about their home. It's also their workplace and their car.
Wendy McLean (31:06): Yes. That's an important one, Isn't it? I always forget about the car, but yes, I've had the window cracked open, it's rained, wet carpet in the car.
Lisa McDonald (31:18): And it's really important. You know, just as a side note there that when those sort of things happens is that is to always be on top of trying to dry things out within 48 hours. So if that means you have to hire an industrial piece of equipment from a remediation group to do that, do it, it's worth it. Because you do not want anything to be wet for more than 48 hours.
Wendy McLean (31:42): Yeah, absolutely. And so you've mentioned that, you know, when helping your patients recovery, you've already mentioned, it's a very much an individual approach. And so what would be some of the interventions that you would use your, nutrients or herbs or lifestyle, and do you work in collaboration with other health professionals as well?
Lisa McDonald (32:03): Yeah, so I guess, because I've been doing this for such a long time, I've really benefited from the training from Dr Shoemaker, but I also incorporate naturopathic philosophy. And also, I'm also really fortunately part of the ISEAI [International Society for Environmentally Acquired Illness], however you want to say that group, which is basically an international group of, I guess thought leaders in this area. And so really tapping into the latest of what, you know, we are finding in practice and some of the research that's being done, et cetera.
So I kind of bring that all together into a kind of like, I guess, a systems based framework in that, you know? So I kind of look at it, bringing all that stuff together. So which I think is really important. Because this is a growing, not growing, that isn’t the right word. It is evolving how we treat these patients and there's more and more research being done to help identify them as well. So it's really important to be on top of that, so of course when I go to treat patients, I look at it from predominantly a systems based framework and then identify where they're at and what's happening to identify the order of things. But mainly, well, the first thing is they have to get away from it; the mould which is probably the most challenging. And then which is probably another conversation or maybe another question I'm not sure because that's a big piece, but I guess secondly, is that we need to make sure that they are eliminating, that their bowels are moving, they're producing bile because we kind of need, because the mycotoxins will circulate through there and we need to be able to get the mycotoxins out as best as possible.
Lisa McDonald (33:34): You need to look at to what extent, how well they are in terms of their detox pathways and in particular glucuronidation, because that's one of the key pathways that where we deal with mycotoxins. We have to look at what you might do with inflammation because there's a lot of a cytokine storm happening. And then the other layer is, is that a part of looking at that individual, often other things come with it, so they might have mast cell activation. They may be more prone to poor metabolism of oxalates and histamines. So you can't just go and throw in a protocol and go, okay, here, have these things off you go. Because a lot of people are sensitive by this stage, by the time they come to me, they're, you know, they can't take a lot of that stuff because they can't, they've got mast cell activation or something like that.
Lisa McDonald (34:40): So you have to take, see where the patient's at. And then the other thing is to often consider yourself as part of a team because they often need broader support. So there's often trauma that either comes with the experience or already there and mental health elements. So that needs supporting. Sometimes they have neural issues, so that needs to be supported. So, you know, having other team members around. That might be acupuncture, or it might be a psychologist, it might be, and so on, bringing the people in as they need. And, and to be honest I remember, you know, one of the things that stood out to me over the years of doing this is that I really noticed that people had done who did work on their psychological or spiritual psycho spiritual. ? re word?
Would that be the word? Psychospiritual side of things actually seems to do a lot better than everybody else. And I think that we now know what that is, and that is about calming down the autonomic nervous system. And so I think that piece of work's really important because that really makes a difference to somebody's recovery. And yeah, I do bring in other practitioners or, you know, work with other health professionals or like that, but also integrated GPs sometimes. So if we feel that they need some pharmaceutical medication, you know, that's where, so, because I think the most important thing is to try and get that person out of where they are, you know, like to pull that person out of the terrible vortex that they're in and move them forward. And if sometimes that means that we have to use things that may not necessarily be considered naturopathic and then you bring on other practitioners, then so be it because sometimes, you know, some of those more pharmaceutical based binders can actually really make a difference in a shorter period of time. And in saying, I'm not saying that it's for everybody because they also have their side effects and their issues and sensitivities with that as well. So again, you have to look the person in front of you, but yes, I do work with other people to get outcomes for the patients.
Wendy McLean (36:55): It's so complex and there's so many challenges in helping these people. And you've mentioned many of them, but what would you say are some of the most challenging? well, the key challenges, I guess, is it having that conversation that they have to move out of their home? Would that be one of the main ones?
Lisa McDonald (37:17): Yes. I, well, I think, well, look, there's multiple. So yeah, I think the fact that your home is, might be making you sick is probably the hardest. And of course, you know, being in lockdown in COVID for the last couple of years has been a little bit challenging in that regard. But also, you know, so people have financial challenges, they have the challenge of the trauma of, and sometimes part of the challenge is actually getting their partners on board or the people in their household on board, because they think they're just crazy people and sometimes and so and are offered, I hate to, it sounds a big accusation, but you know, sometimes they also get gas lit a bit because I'll go to different practitioners and they'll go, oh, it's all on your head. And so, you know, validation's important. But yeah, some of the, a lot of the challenges tend to be how big it is to move out of their place. Financial challenges. Support challenges and you know, for those people that are in rentals, I mean, that's another layer as well because you've got landlords that go, oh, well you are the one who caused the mould because you haven't maintained the place or we'll just send someone in and they just come in and just wipe it off the walls and paint over it. And off you go. And it's like, oh my God. You know? So you know, so because it's not a recognised illness in Australia at the moment, it does present that challenge in, in that they don't necessarily get the support that's required.
Wendy McLean (38:53): Yeah. I understand. And I've unfortunately, as a renter I had that experience with the landlord as well and had to move out of my place immediately as they unearthed black mould when they were ripping out the bathroom. So I can empathise with people going through this experience as well.
Lisa McDonald (39:12): You poor thing that's not good.
Wendy McLean (39:13): Yeah. So look, there has been a Senate inquiry into CIRS in 2018. But do you think this has led to any changes in our current clinical practice and, or do you think, you know, we've still got a long way to go to getting this recognised in conventional medical practice?
Lisa McDonald (39:31): Look, I think the inquiry was a step in the right direction. It was, we were so fortunate for it to occur and a lot of that was well, some of it was driven too because we've had MPs in parliament actually get CIRS and that sort of helped to facilitate some of that. But, you know, and then we had COVID. So we started a momentum and then we had COVID, but it was a step in the right direction. I think there's some challenges we've still got to get through to, for it to be recognised. Fortunately, the government did provide some support for research in this area back in, I think they were in 2020/21, the last two years are a blur. But so there is some research underway, you know, linking in with some integrative GPs that are working in this area.
Lisa McDonald (40:21): There's also been some other repeats of research done by other professions around building structures and things like that. So the research is on the way to sort of get us to a place where it can be recognised. But, you know, as with a lot of things, you see things in clinical practice, there's research that's done, and then there's another five or ten years maybe before it might actually change, the ways that things happen and that's for all sorts of reasons. So I think that we've probably got some years ahead before it actually gets recognised, but at least it's a step in the right direction. And I'm actually, it's actually terrible on one respect that we're all having this mould problem, but the silver lining in that is that, is that because it's such a problem that perhaps it'll rise to the surface a little bit quicker than perhaps if we didn't have such a large proportion of the population potentially unwell. So I think that, you know, perhaps it'll happen sooner than expected, but yeah, we're on the way.
Wendy McLean (41:29): Yeah. And I mean, definitely I think it's certainly been highlighted in the press over the last few months, which I think yes is good or some misinformation, but a lot of good information out there as well. And so I think just getting that information out there, educating people is critical as well. So on that note, where can practitioners and the general public find out more information about mould illness and mould?
Lisa McDonald (41:56): Well, they can probably go to my website. I've got two websites. One is my name, lisamcdonald.com.au and the other one is indigosagehealth.com.au. And on those sites, they'll find some resources around symptoms, et cetera, and also how I practice.
Wendy McLean (42:13): Yeah. Fantastic. And we can put some links to those on, on the site as well. Well, that's been really informative. Thank you so much for sharing your personal experience and also your years of clinical experience with us. And I'm sure there's a lot of practitioners and patients out there who'll get a lot out of this. So thank you. We really appreciate you joining us today.
Lisa McDonald (42:37): My pleasure, Wendy
Wendy McLean (42:39): And thanks to you for tuning into this episode. We appreciate your support and feel free to leave us a review. We'd love to hear from you. Thank you.