Chronic lung disorders, such as asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis (CF) and idiopathic pulmonary fibrosis (IPF) are usually accompanied by intestinal symptoms which imply the existence of an immunological link between the gut and the lungs. This link is referred to as the gut-lung axis (1). The composition of the gut microbiota affects immune responses and development of inflammation, not only in the gastrointestinal tract but also in distal sites such as the lungs (2).
The existence of microbial organisms in the lungs, referred to as the lung microbiome, has recently been discovered leading to research into their effect on lung function and disease. Changes in gut microbiota could affect lung microbiota, and vice versa (3). Dysbiosis in gut and lung microbiota have been linked to increased incidence and severity of asthma, allergy, CF, COPD and respiratory infections (1,4,5).
A healthy gut microbiota maintains homeostatic local immune responses through the exposure of structural ligands (e.g. lipopolysaccharide) and secreted metabolites (e.g. short-chain fatty acids). Invading microorganisms and absorbed metabolites influence circulating lymphocytes and contribute to the regulation of the systemic immune responses. Gut microbiota dysbiosis results in altered microbiota-derived signals which lead to a changed immune response. In early life, when the immune system is still developing, this disturbance can substantially alter the way in which the immune system perceives its surroundings in later life, which can lead to the development of chronic inflammatory disorders in the gut and lung. In adulthood, dysbiosis of the gut microbiota (e.g. exposure to cigarette smoke) can cause systemic inflammation and an overgrowth of opportunistic pathogens which can lead to chronic inflammation in the lungs (5). Exacerbations of chronic lung diseases occur as an uncontrolled and inappropriate inflammatory response regulated in part by the gut microbiota (2).
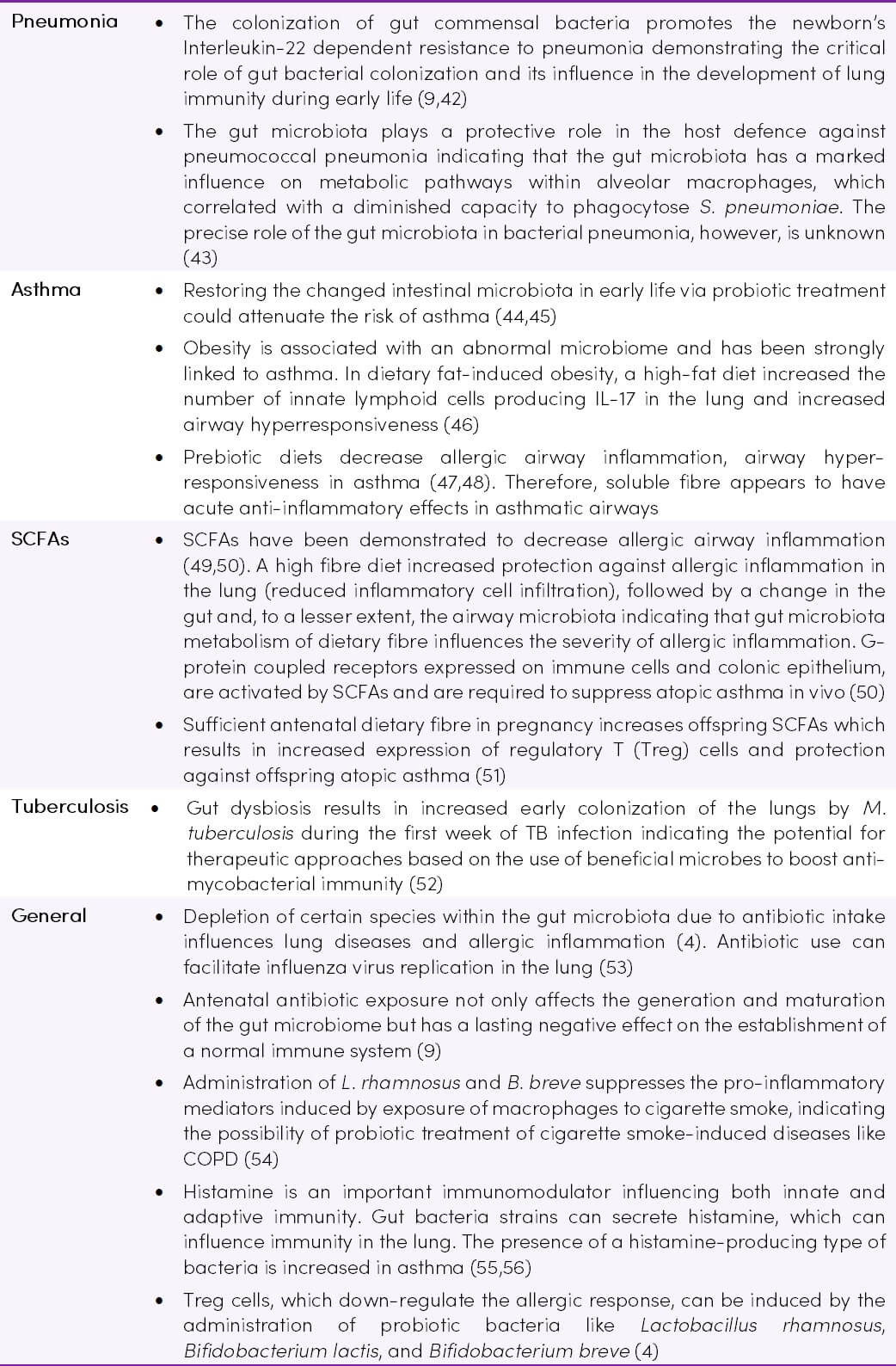
The gut microbiome communicates with the lung via multiple bi-directional pathways (Figure 1) and commensal gut microbiota appear to be critical in lung defence against bacterial invasion (2,6).
Figure 1. Gut-lung communication (7) CC BY 4.0
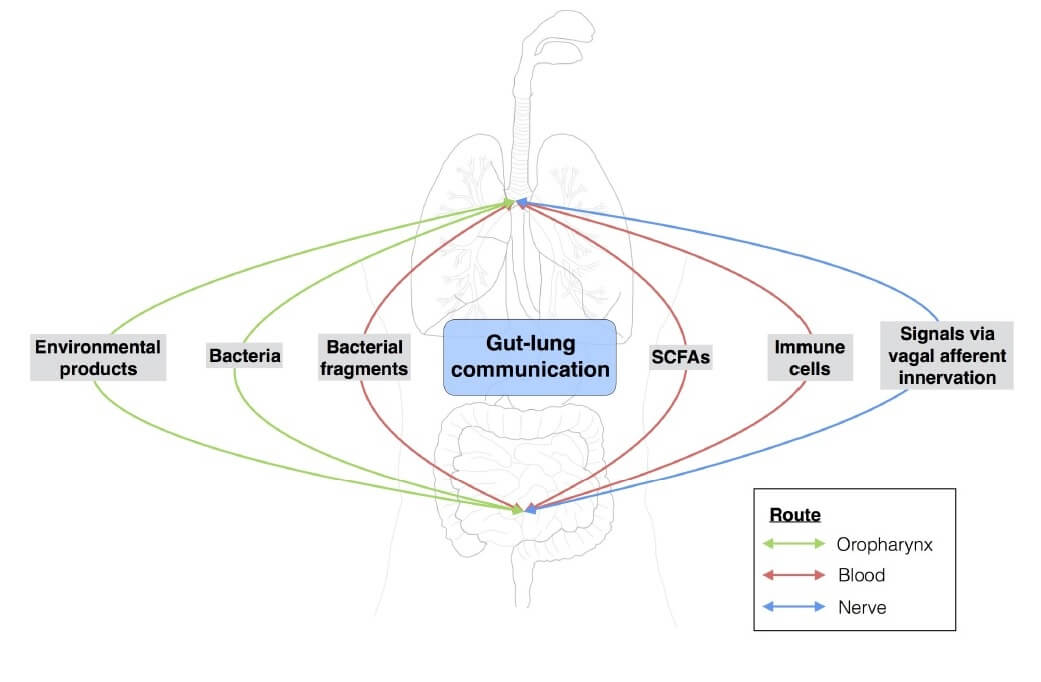
Research into the gut-lung axis is still in its infancy, but it may potentially serve as a new direction for lung disease treatment, with some of the existing probiotic strains showing beneficial effects on lung health (4,5). A better understanding of microbiome interactions with inflammation and other major risk factors for chronic lung disease such as host genetics and cigarette smoking (Figure 2) will aid in optimising current treatments and in managing chronic lung conditions.
Figure 2. Risk factors for chronic respiratory diseases and associated pathology with microbiome. Adapted from (8) CC BY-NC-ND 4.0
Traditional Understanding
Historically, traditional culture-based studies and classic teaching indicated that normal lungs are free from bacteria, and this notion has persisted in contemporary medicine (1). Recent evidence has identified microbial organisms in the lungs in healthy individuals (the lung microbiome).
The lung microbiome
In humans, lung microbiota have been identified in healthy donors and in patients with chronic lung disease (1). The total number of bacteria in lung tissue is relatively small compared with that of gut microbiota. As with the gut microbiome, the lung microbiome is considered to be important to immunity by priming the immune system. Dysbiosis in the lung predisposes to the development of respiratory disease and may be relevant in the aetiology and/or progression of chronic lung diseases (1,9). It is not clear whether dysbiosis is a cause or a consequence of immune dysregulation and disease initiation or progression. Further study of the relationship between lung microbiota and respiratory disease might result in future manipulation of lung microbiota as a rational and promising therapy (1). It has been suggested that exacerbations of chronic lung disease are more likely due to episodes of dysbiosis of the microbial ecosystem of the respiratory tract rather than infection (2).
There are many factors, such as anatomical injuries, pathological effects, physiological changes and immune system defects which could disrupt the lung microbiota and result in chronic lung diseases (1). The influence of gut microbiota on lung immunity has been recently explored. Changes in the gut microbiome have been linked with lung immunity and clinical outcomes in chronic respiratory diseases. Conversely, the lung microbiota also influences the gut microbiota through the bloodstream (2).
Latest Research
Asthma
Asthma is a chronic and multifactorial disease thought to be caused by a combination of genetic and environmental factors including air pollution and allergens.
The lung microbiome is altered during the development of allergic asthma and it has been suggested that both the gut and lung microbiota, as well as the local and systemic immune response, play a role in predisposing an individual to asthma (10).
Lung microbiome and asthma
- The composition of lung microbiota in individuals with asthma is different from healthy controls (1). The underlying inflammation in atopic asthma appears to be related to the lung microbiota composition (2,11).
- Treatment with inhaled corticosteroids is associated with changes in the airway inflammatory response to microbiota (12,13).
Gut microbiome and asthma
A correlation has been demonstrated between gut microbial diversity and asthma.
- Several maternal factors are associated with childhood asthma risk (Figure 3).
- Infant antibiotic use during the first year of life is the greatest predictor of childhood asthma (14,15).
- Colonization with fewer bacteria species during the first month of life is associated with an asthma diagnosis at age 7 (16).
- There appears to be a critical window of colonization that occurs during early infancy in which gut microbial communities shape immune maturation and confer susceptibility to allergic airway inflammation (17). Studies have examined gut microbiota maturation over the first year of life in infants at high risk for asthma, and whether it is modifiable by early-life Lactobacillus supplementation (18). Results showed that early-life gut microbial development is distinct, but plastic, offering a novel strategy for early-life preventive interventions.
- Adults with long-term asthma were found to have a decreased abundance of Bifidobacteria (19).
- Faecal microbial transplant therapy for asthma may represent a therapeutic approach in the foreseeable future (20).
Figure 3. Early life factors influencing gut microbial composition and risk of allergy and asthma (15,21,22,23,24).
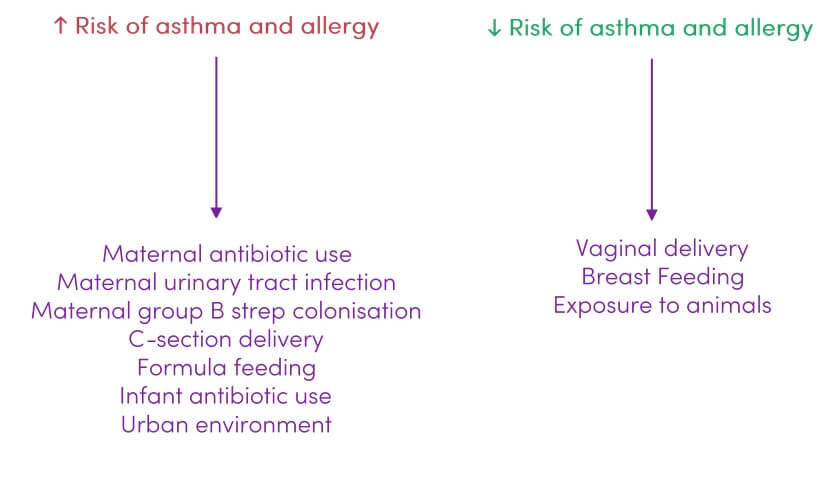 The idea of primary prevention of asthma and allergy by manipulation of environmental microbial exposures seems a very promising approach. The first months of life, or even the prenatal period, seem to be the most sensitive for effective intervention. Identification of individuals with a high asthma risk at this early stage would be very important (25). A better understanding of microbiome-driven pathophysiology and inflammation, in conjunction with the interaction of major risk factors for asthma development, such as host genetics and tobacco smoke, would aid in optimizing current treatments and in managing this chronic lung condition (26).
The idea of primary prevention of asthma and allergy by manipulation of environmental microbial exposures seems a very promising approach. The first months of life, or even the prenatal period, seem to be the most sensitive for effective intervention. Identification of individuals with a high asthma risk at this early stage would be very important (25). A better understanding of microbiome-driven pathophysiology and inflammation, in conjunction with the interaction of major risk factors for asthma development, such as host genetics and tobacco smoke, would aid in optimizing current treatments and in managing this chronic lung condition (26).
The Hygiene Hypothesis and Asthma
An association between decreasing frequency of childhood infections and the increasing development of asthma and allergies has been recognized for years, giving rise to the hygiene hypothesis: that a decrease in infectious exposures early in life (due to improved hygiene, sanitation, cleaner homes and environments) results in deranged mucosal tolerance and increased autoimmune pathology. Early bacterial stimulation appears to reduce asthma susceptibility by helping the immune system develop lifelong tolerance to innocuous antigens (2). Hygiene-associated deviations in gut microflora composition may be the environmental factor underlying the development of atopy and asthma in genetically predisposed individuals (27).
Several cross-sectional studies in different countries have compared the prevalence of asthma, hay fever and allergic sensitization in children living in farming and non-farming environments. They showed that children born and raised in a farming environment were less prone to the development of atopic symptoms and asthma later in life. This protective effect was even stronger in adults that had remained in the farming environment. These observations support the hypothesis that exposure to a wide range of diverse microbial signals during the first few months of life has a major impact on susceptibility to the development of asthma (7).
Chronic Obstructive Pulmonary Disease
COPD is a type of obstructive lung disease characterized by long-term poor airflow. The gut and lung microbiota contribute to the pathogenesis and exacerbations of COPD. Studies indicate that bacterial colonization in the lung is associated with a chronic bronchitic phenotype with an increased risk of exacerbations and accelerated loss of lung function.
Once innate lung defence mechanisms are disrupted by an initiating factor (e.g. smoke exposure or air pollution) the microbiome in the airway is disrupted which drives inflammatory processes in COPD, causing progressive airflow obstruction and parenchymal damage (2).
Evidence indicates that bronchus protection is a consequence of antigen handling in the gut via T cell-dependent recruitment and activation of neutrophils and secretion of antibacterial factors (2).
The lung microbiotas in patients with mild and moderate COPD are similar to the lung microbiota in healthy controls. The change of lung microbiota may only be found in patients with advanced COPD (10).
Cystic Fibrosis
Cystic fibrosis (CF) is an inherited disorder that mainly affects the lungs and is characterised by a build-up of thick, intransient mucus linings of the digestive and respiratory mucosa. The syndrome of CF in the lungs displays a progressive development of bronchiectasis ![]() and obstructive lung disease. The relationship between lung microbiota and the pathogenesis of CF is still controversial, however, the gut microbiota is considered as a link in CF.
and obstructive lung disease. The relationship between lung microbiota and the pathogenesis of CF is still controversial, however, the gut microbiota is considered as a link in CF.
- Gut microbiota and their metabolites can influence host metabolism and immune function, which are heavily implicated in CF progression and comorbidity management (28). Individuals with CF display a significantly altered gut microbiota, including reduced microbial diversity compared to healthy controls (29).
- Intakes of some dietary flavonoids may be associated with gut microbiota variations with potential consequences for metabolism, immune function, and inflammation, which are important in CF lung disease and co-morbidity management (28).
- Limited preliminary studies have shown that oral probiotics may help reduce the frequency of pulmonary exacerbation and associated hospital admissions, as well as gut inflammation and discomfort in children and adults with CF (30,31,32,33,34).
- The use of probiotics is rational and has been in practice since the 1980s, despite the paucity of supporting evidence and lack of specific guidelines (31).
- Vitamin D status may be essential for the development of a healthy gut microbiome, particularly in conditions defined by chronic mucosal inflammation such as CF. It has been suggested that using high dose vitamin D may be used to favourably alter the aberrant mucosa seen in patients with CF. This may result in improved clinical outcomes in association with a low inflammatory environment that allows beneficial bacteria to outcompete opportunistic pathogens. Vitamin D also potentially plays a role in pulmonary function (35).
Tuberculosis
- Tuberculosis (TB) outcomes can be affected by gut microbiota. Maintaining homeostasis of gut microbiota may be beneficial for recovery and prevention of recurrence of tuberculosis infection (36).
- The cross-talk between the lung and gut microbiome, as well as innate and adaptive immune cells that may link these two mucosal sites, appear to be important in the prevention, pathogenesis, and treatment of TB (37).
- Narrow-spectrum, first-line anti-TB drugs have dramatic effects on microbiome diversity and immunity, which persists even after the completion of TB drug therapy (38,39). The persistent dysbiosis that accompanies curative anti-TB treatment could contribute to post-treatment susceptibility to mycobacterial reinfection, as well as infection with other diseases linked with altered immune responses (40,41).
Experimental Studies
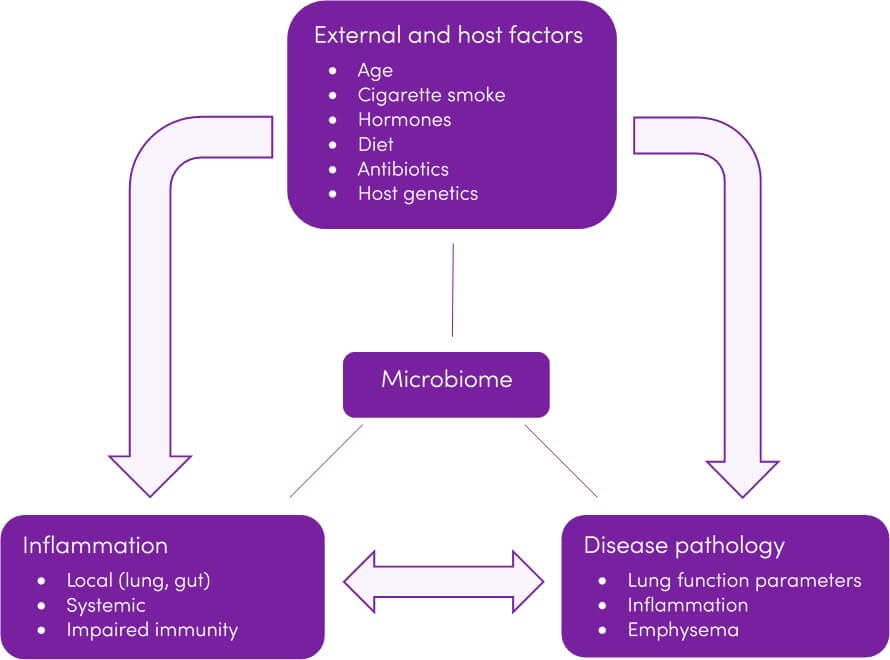
Recent experimental studies are summarised in Table 1.
Table 1. Recent experimental studies involving the gut-lung axis